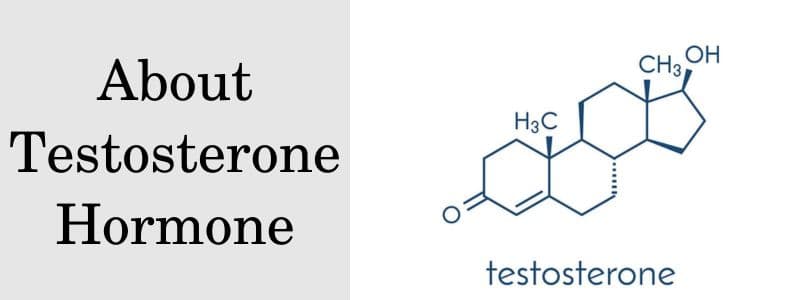
Testosterone is a vital hormone, predominantly associated with the development and regulation of male characteristics and reproductive activities, although it is also present in females in smaller amounts. This steroid hormone, part of the androgen group, plays a crucial role in the human body, influencing a range of physiological and psychological functions.
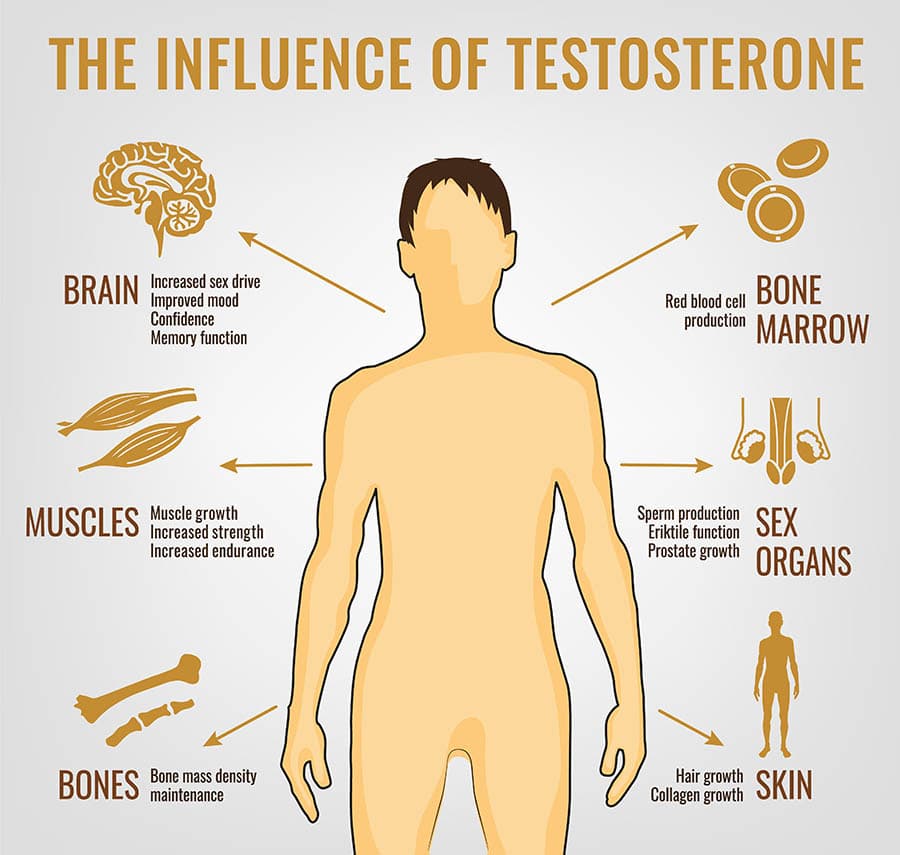
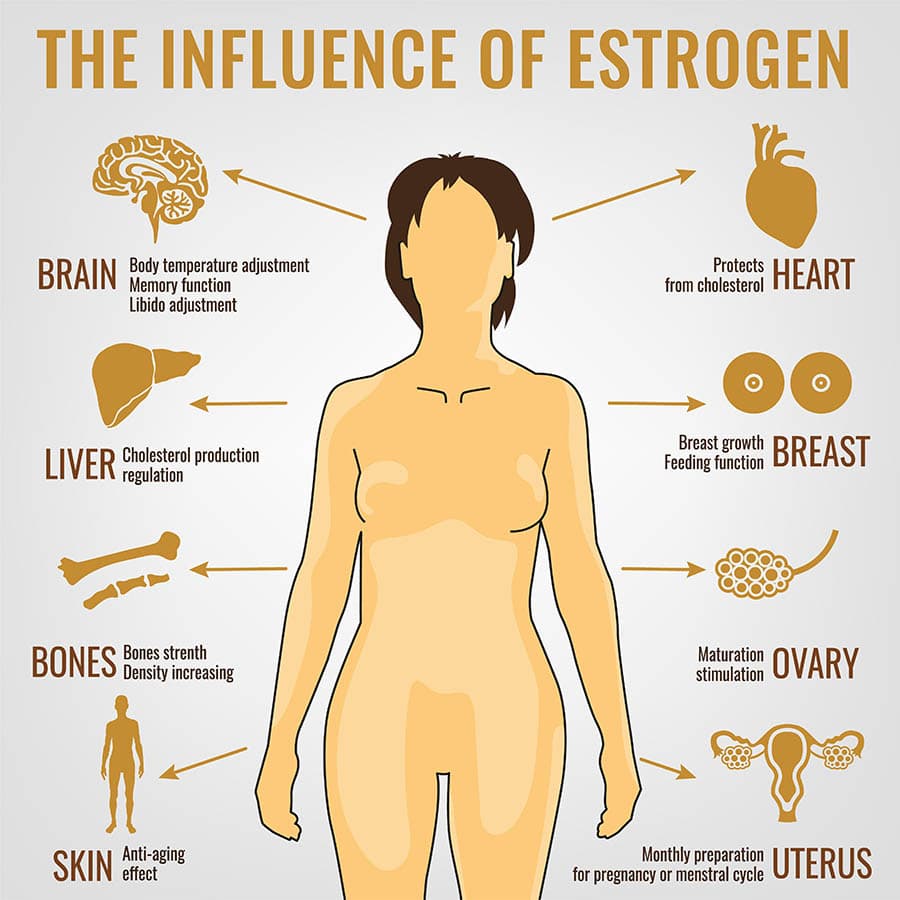
In both sexes, testosterone has significant effects beyond reproductive tissues. It plays a role in bone density, muscle strength, and mass, and is also believed to influence mood, energy levels, and cognitive functions. The hormone has a role in the regulation of libido (sex drive) in both males and females.
Production and Regulation of Testosterone
The production and regulation of testosterone, a critical hormone in the human body, are complex processes involving multiple organs and regulatory systems.
How is testosterone synthesized?
Testosterone is synthesized primarily in the Leydig cells of the testes in males and, to a lesser extent, in the ovaries and adrenal glands in females. The biosynthesis of testosterone starts from cholesterol, which undergoes a series of enzymatic transformations.
In males, the process is stimulated predominantly by the luteinizing hormone (LH) released from the anterior pituitary gland. In females, although the mechanism is similar, the quantity produced is considerably less.
How does testosterone regulate?
The regulation of testosterone production is primarily controlled by the hypothalamic-pituitary-gonadal (HPG) axis through a feedback loop:
- Gonadotropin-Releasing Hormone (GnRH) Secretion: The hypothalamus secretes GnRH, which signals the pituitary gland to release LH and follicle-stimulating hormone (FSH).
- Luteinizing Hormone (LH) Stimulation: LH is the key hormone that stimulates Leydig cells in the testes to produce testosterone. In females, LH influences testosterone production in the ovaries and adrenal glands.
- Feedback Mechanism: Elevated levels of testosterone exert negative feedback on the hypothalamus and pituitary gland, reducing the secretion of GnRH and LH, thereby regulating its own production.
Factors Affecting Testosterone Levels
Several factors can influence testosterone levels, including:
- Age: Testosterone levels naturally decline with age.
- Circadian Rhythms: Testosterone levels typically peak in the morning and decline throughout the day.
- Lifestyle Factors: Diet, exercise, stress, and sleep can all impact testosterone levels.
- Health Conditions: Certain medical conditions, such as hypogonadism, and medications can affect testosterone production.
Understanding the production and regulation of testosterone is crucial for diagnosing and treating conditions related to hormonal imbalances. Ongoing research continues to shed light on this complex endocrine process, enhancing our ability to manage related health issues effectively.
Functions of Testosterone in the Body
Testosterone, a key hormone in the human body, has a wide range of functions affecting both physical and mental health. It is critical in both males and females, although its presence is much higher in males.
Physical Development in Males
In males, testosterone is the principal hormone responsible for the development of male reproductive tissues, such as the testes and prostate, as well as secondary sexual characteristics. These include increased muscle and bone mass, deepening of the voice, and growth of body hair.
Muscle Mass, Bone Density, and Body Composition
Testosterone plays a crucial role in muscle growth, bone density, and the overall body composition in both sexes. It increases muscle protein synthesis and promotes the growth of muscular tissue. Additionally, it contributes to bone density and strength, reducing the risk of osteoporosis.
Sexual Function and Reproductive Health
Testosterone is essential for maintaining sexual function and reproductive health. In males, it regulates libido (sex drive), erectile function, and spermatogenesis. In females, although present in smaller amounts, it also contributes to sexual arousal and may play a role in ovarian function.
Mood and Mental Health
Testosterone has been linked to mood regulation and mental health. It is thought to influence feelings of well-being, energy levels, and may play a role in the prevention of depression and cognitive decline.
Metabolic and Cardiovascular Health
Testosterone influences several metabolic processes. It helps regulate the distribution of body fat and is involved in cholesterol metabolism. Additionally, adequate levels of testosterone are important for cardiovascular health.
Understanding the multifaceted roles of testosterone in the body is crucial for diagnosing and managing a range of health conditions. It highlights the hormone’s significance beyond just reproductive health, underscoring its importance in overall physical and mental well-being.
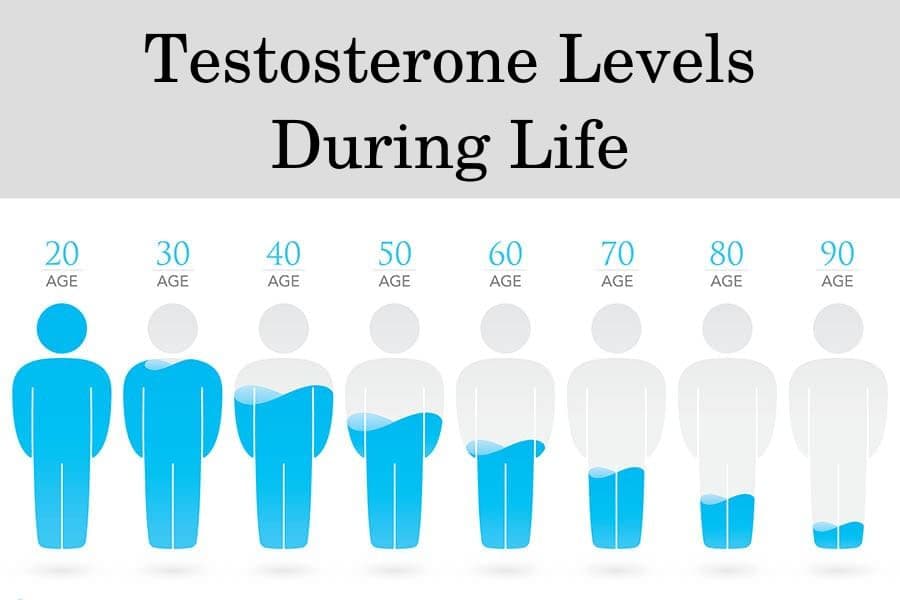
Changes in Testosterone Levels During Life
Testosterone levels vary significantly throughout an individual’s life, influencing various physiological and psychological aspects at each stage. Understanding these variations is crucial in assessing health and diagnosing potential hormonal imbalances.
Testosterone Levels During Childhood and Adolescence
In males, testosterone levels are relatively low in childhood. However, during puberty, there is a significant surge in testosterone, triggering the development of secondary sexual characteristics, such as increased muscle mass, deepening of the voice, and growth of facial and body hair. This surge also contributes to the growth spurt typically observed during adolescence.
Testosterone Levels During Early Adulthood
Testosterone levels peak in early adulthood (ages 20-30). During this phase, the hormone is crucial for maintaining muscle strength, bone density, and a healthy libido. It also plays a role in general well-being and mood regulation.
Testosterone Levels During Midlife and Aging
As men age, particularly after the age of 30, testosterone levels gradually decline at a rate of about 1% per year. This decline can lead to changes in sexual function, mood, energy levels, and body composition, such as decreased muscle mass and increased body fat. In women, testosterone levels also decline with age, especially after menopause, impacting libido and bone density.
Testosterone Levels During Andropause or Late-Onset Hypogonadism
In some men, the decrease in testosterone can be more significant, leading to a condition often referred to as andropause or late-onset hypogonadism. Symptoms may include reduced libido, erectile dysfunction, fatigue, depression, and cognitive decline.
Testosterone Levels in Females
In females, testosterone plays a role in ovarian function, bone strength, and sexual well-being. Levels peak in the mid-20s and decline gradually, with a more notable decrease during and after menopause, which can affect sexual desire, mood, and physical strength.
Understanding the variations in testosterone levels throughout different life stages helps in identifying and managing conditions related to hormonal imbalances. It also underscores the importance of considering age-related hormonal changes in both diagnostic and therapeutic contexts.
Causes and Symptoms of Testosterone Imbalance
Testosterone imbalance, encompassing both high and low levels of the hormone, can lead to various health issues in both males and females. Recognizing the causes and symptoms of these imbalances is crucial for effective diagnosis and treatment.
High Testosterone Levels
Elevated testosterone levels are less common and can be caused by several factors, including:
- In Males: Conditions like testicular tumors or adrenal gland disorders.
- In Females: Polycystic ovary syndrome (PCOS) is a common cause of increased testosterone levels.
- External Factors: Anabolic steroid use can also lead to abnormally high testosterone levels.
Symptoms of high testosterone:
- In males: Aggressiveness, acne, and an increased risk of liver disease.
- In females: Irregular menstrual cycles, increased body hair, and a deeper voice.
Low Testosterone Levels
Low testosterone levels, or hypogonadism, can result from various causes:
- Primary Hypogonadism: Direct testicular failure due to conditions such as Klinefelter syndrome or testicular trauma.
- Secondary Hypogonadism: Failure of the hypothalamus or pituitary gland to signal the testes, due to conditions like pituitary tumors or inflammatory diseases.
Symptoms of low testosterone:
- Reduced libido, erectile dysfunction, decreased muscle mass and strength.
- Fatigue, depression, and cognitive difficulties.
- Osteoporosis or reduced bone density.
Diagnosis of Testosterone Deficiency
Diagnosing testosterone imbalance involves clinical evaluation and blood tests to measure hormone levels. It’s important to interpret these results in the context of the patient’s overall health and symptoms.
The accurate diagnosis of conditions related to testosterone levels is essential for effective treatment and management. A comprehensive approach combining clinical evaluation, symptom assessment, and laboratory testing is required.
1. Clinical Evaluation
The first step in diagnosing testosterone-related conditions involves a thorough clinical evaluation. This includes:
- Medical History: Gathering information on symptoms, family history, past medical conditions, and any medications or supplements being used.
- Physical Examination: Assessing physical signs that might indicate testosterone imbalance, such as changes in body hair distribution, muscle mass, and testicular size in males.
2. Symptom Assessment
Symptoms can vary widely depending on whether testosterone levels are high or low and can differ between males and females. Common symptoms to assess include:
- For Low Testosterone: Decreased libido, erectile dysfunction, fatigue, muscle weakness, and mood changes.
- For High Testosterone: In males, symptoms might include acne, aggressive behavior, and infertility. In females, symptoms can include hirsutism, acne, and menstrual irregularities.
3. Laboratory Testing
Blood tests are the most reliable method for measuring testosterone levels:
- Total Testosterone Levels: This test measures both free and bound testosterone in the blood. It’s the primary test for diagnosing testosterone imbalance.
- Free Testosterone Levels: Sometimes, measuring only free testosterone (the biologically active form) can be helpful, especially in cases where total testosterone levels are borderline.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) Levels: These tests can help differentiate between primary (testicular) and secondary (hypothalamic or pituitary) causes of testosterone abnormalities.
Considerations in Testosterone Testing:
- Timing of Blood Samples: Testosterone levels can fluctuate throughout the day. Levels are typically highest in the morning.
- Repeat Testing: Due to variability, repeat testing is often recommended to confirm initial findings.
- Age-Adjusted Reference Ranges: Testosterone reference ranges can vary by age, and this should be considered when interpreting results.
Diagnosing testosterone-related conditions requires careful evaluation of both clinical and laboratory data. Understanding the nuances of testosterone testing and interpretation is crucial for endocrinologists and healthcare providers in providing accurate diagnoses and effective treatment plans.
How to treat testosterone deficiency
If testosterone deficiency is suspected based on symptoms, we will order a simple blood test to measure the patient’s serum total testosterone level. In addition, we may order tests for free testosterone and sex hormone-binding globulin levels to gain more insight.
Testosterone levels do naturally decrease modestly with aging, so it’s important to compare the patient’s results to normal healthy ranges based on age. Significant drops below those expected ranges can confirm testosterone deficiency.
Treatment Options
If testosterone deficiency is diagnosed, we develop an appropriate treatment plan for the patient. The main treatment options include:
- Testosterone replacement therapy: This involves supplementing testosterone via injections, transdermal gels/patches, or pellets implanted under the skin. It effectively alleviates symptoms in most men. Therapy is continued indefinitely unless testosterone levels normalize or side effects occur.
- Lifestyle changes: Losing weight, improving diet, exercising regularly, reducing stress, and getting quality sleep can all help boost natural testosterone production. These should be encouraged regardless.
- Medications: Certain antidepressants, corticosteroids, and opioid pain medications can suppress testosterone, so adjustments may be made to those if applicable.
We monitor patients on testosterone replacement therapy by ordering follow-up blood tests and assessing their symptomatic response. Dosages are adjusted accordingly to keep testosterone levels in an optimal range while avoiding excess levels.
If therapy remains effective with no issues, patients often enjoy significantly improved energy, sex drive, body composition, and quality of life.
What are the risks and contraindications for testosterone therapy?
While TRT can be an effective treatment for low testosterone levels, it is not without risks and considerations. Understanding these potential risks and carefully monitoring patients is crucial for safe and effective therapy. This section outlines the key risks and considerations associated with testosterone therapy.
Cardiovascular Risk
There is ongoing debate and research regarding the association between testosterone therapy and cardiovascular risk. Some studies suggest an increased risk of heart attack and stroke, particularly in older men or those with pre-existing heart conditions.
Prostate Health
Testosterone can stimulate the growth of prostate tissue. Therefore, there is concern about the potential for TRT to exacerbate prostate cancer or benign prostatic hyperplasia (BPH). Regular prostate monitoring, including PSA testing, is recommended during testosterone therapy.
Polycythemia
TRT can lead to an increase in red blood cell production, known as polycythemia. This condition can increase the risk of blood clots, posing a significant health risk, particularly in patients with a history of thrombosis.
Sleep Apnea
Some evidence suggests that testosterone therapy may worsen sleep apnea, a condition characterized by pauses in breathing during sleep. Patients with pre-existing sleep apnea should be closely monitored during TRT.
Impact on Fertility
Testosterone therapy can suppress sperm production, potentially affecting fertility. Men wishing to father children should discuss alternative treatments or fertility preservation strategies with their healthcare provider.
Liver Function
Oral testosterone preparations, though less commonly used, can have adverse effects on liver function. Monitoring liver enzymes is recommended for patients on any form of testosterone therapy, particularly oral formulations.
Mental Health Effects
While testosterone therapy can improve mood and energy levels, its impact on mental health is complex. Mood swings, aggression, and other psychological effects have been reported in some cases.
Testosterone therapy requires careful consideration of the potential risks and regular monitoring to ensure patient safety. A personalized approach, taking into account each patient’s unique medical history and health goals, is essential for optimal treatment outcomes.
FAQ About Testosterone
Q: Can women have testosterone imbalances?
A: Yes, women can have imbalances in testosterone levels, though they naturally have lower levels than men. Imbalances can affect menstrual cycles, fertility, mood, and bone strength.
Q: How is testosterone measured?
A: Testosterone levels are measured through blood tests, which should ideally be conducted in the morning when testosterone levels are highest.
Q: Is testosterone therapy safe?
A: Testosterone therapy can be safe when appropriately prescribed and monitored by a healthcare provider. It’s important to understand the potential risks and benefits, which can vary based on individual health conditions.
Q: Can lifestyle changes affect testosterone levels?
A: Yes, lifestyle factors like diet, exercise, stress management, and sleep can influence testosterone levels. Maintaining a healthy lifestyle can support healthy hormone levels.
Q: Are there natural ways to boost testosterone?
A: Regular exercise, particularly strength training, a balanced diet, adequate sleep, and stress reduction can naturally help maintain or boost testosterone levels.
Conclusion
Testosterone, a vital hormone in the human body, plays a crucial role in a variety of bodily functions, from sexual development and reproductive health to mood regulation and bone density. Understanding the nuances of testosterone levels, how they can become imbalanced, and the implications of these imbalances is important for overall health.
Whether addressing low testosterone levels or managing conditions related to high testosterone, it’s important to approach treatment and management with a comprehensive understanding of the individual’s overall health, lifestyle, and specific symptoms. The role of lifestyle modifications, alongside medical interventions, cannot be overstated in managing testosterone levels.
For individuals experiencing symptoms or concerns related to testosterone, consultation with healthcare professionals, specifically endocrinologists, is key. They can provide personalized advice, conduct necessary testing, and develop a treatment plan that aligns with the individual’s health needs and goals.